Are you tired of slow, error-prone claims processing that frustrates customers and drains resources? What if AI in insurance could transform the entire process, making it faster, more accurate, and fraud-resistant? In this post, we’ll dive into how AI-driven automation is revolutionizing claims handling—helping insurers cut costs, detect fraud early, and improve customer satisfaction. Let’s unpack how AI empowers insurance companies to work smarter, not harder.
Claims Fraud Detection: Enhancing Accuracy and Security
Claims fraud has long been a costly burden on insurance providers, accounting for billions of lost dollars annually. Traditional detection methods often rely on manual reviews or rule-based systems, which can be slow, inconsistent, and prone to false positives. This is where AI in insurance, particularly in claims fraud detection, offers a powerful leap forward.
AI models use advanced machine learning algorithms and anomaly detection techniques to analyze vast datasets, including claim submissions, historical claim records, customer behavior, and external data sources. Unlike human investigators, AI can detect subtle patterns and irregularities that suggest fraudulent activity but may be invisible to the naked eye.
For example, AI can identify common fraud schemes such as staged accidents, duplicate claims, inflated repair costs, and falsified injury reports. By cross-referencing data points such as geolocation, timing, policyholder activity, and social media inputs, the system flags suspicious cases for further investigation.
The benefits to insurers are substantial:
- Risk Reduction: AI reduces exposure to fraudulent claims by enabling earlier and more accurate identification of suspicious activity.
- Cost Savings: Minimizing fraud lowers claim payouts and administrative expenses, improving overall profitability.
- Improved Trust: Customers appreciate fair, transparent claims processing and are less likely to experience wrongful denials or unnecessary delays.
Several global insurers in 2025 are leveraging AI-powered fraud detection platforms that continuously learn from new fraud patterns, adapting in real time to emerging schemes. This adaptive capability helps maintain high detection accuracy and reduces false positives that can frustrate honest claimants.
Practical Tip:
To maximize the effectiveness of AI-based fraud detection, insurers should integrate diverse data sources and continuously retrain models, ensuring detection algorithms remain current with evolving fraud tactics.
Process Automation: Streamlining Claims Handling for Efficiency
AI in insurance extends beyond fraud detection into broad process automation, transforming how claims are handled from start to finish. Traditionally, claims processing involved manual data entry, validation, underwriting review, and customer communication—tasks that are repetitive, error-prone, and time-consuming.
By automating these workflows through AI, insurance companies can accelerate claim adjudication without sacrificing accuracy. Key areas of process automation include:
- Data Extraction: AI-powered optical character recognition (OCR) and natural language processing (NLP) extract relevant information from submitted documents such as photos, invoices, and police reports, dramatically reducing manual input.
- Claim Validation: Machine learning algorithms cross-check claimant details, policy coverage, and historical data to validate claim legitimacy and flag inconsistencies automatically.
- Customer Communication: Chatbots and virtual assistants powered by AI engage with claimants directly, providing status updates, gathering supplementary information, and answering routine queries 24/7.
In 2025, robotic process automation (RPA) platforms combined with sophisticated NLP engines enable end-to-end claims lifecycle automation. This integration eliminates bottlenecks caused by paper-based forms and human delays, improving cycle times from days to hours or minutes.
Automation also enhances workflows by reducing errors caused by fatigue or manual oversight. This means claims handlers can prioritize complex cases requiring human judgment while routine claims are processed swiftly by AI systems.
Another benefit of process automation is scalability. During catastrophe claims surges—such as natural disasters—AI platforms can instantly handle high volumes with consistent quality, preventing backlog and customer dissatisfaction.
Practical Tip:
Insurers should map their claims workflows carefully to identify high-impact automation targets, then pilot AI tools in those areas before scaling across the enterprise. Continuous monitoring and feedback loops are essential for sustained performance improvements.
Integrating AI in Insurance Claims Systems
Implementing AI in insurance claims processing requires a strategic approach to ensure smooth integration, minimal disruption, and measurable ROI. Insurers must approach AI not as a plug-and-play solution but as a technology layered onto existing infrastructure.
Successful AI integration involves:
- Assessment and Planning: Analyze existing claims systems and workflows to identify automation opportunities, data availability, and technology gaps.
- Data Quality & Management: High-quality, clean data is critical for AI accuracy. Invest in data cleansing, normalization, and governance frameworks upfront.
- Incremental Deployment: Start with pilot projects targeting specific claims processing stages (e.g., initial claim intake or fraud detection) to validate methods before broader adoption.
- Technology Stack Alignment: Choose AI tools compatible with legacy systems or plan phased upgrades to cloud-based platforms for greater scalability and flexibility.
- Workforce Enablement: Train claims teams on AI tools, emphasizing collaboration between human expertise and AI insights rather than replacement.
Anticipating challenges is key. Data silos, legacy system constraints, and integration complexities can slow progress. Furthermore, ensuring compliance with insurance regulations and data privacy laws (such as GDPR or HIPAA where applicable) is critical.
The AI shift also necessitates a workforce transformation. Roles will evolve as employees transition from routine processing to more analytical, decision-making functions. This requires upskilling and change management to minimize resistance.
Practical Tip:
Engage cross-functional teams—including IT, claims operations, legal, and HR—early in the AI integration roadmap to balance technical feasibility, regulatory compliance, and human factors.
Future Trends and Innovations in AI for Insurance Claims
Looking ahead, AI in insurance claims processing will become even more sophisticated, driven by advances in deep learning, predictive analytics, and ethical AI frameworks.
Some emerging trends include:
- Deep Learning for Complex Pattern Recognition: Neural networks will improve the accuracy of claims assessments by analyzing unstructured data like images and voice recordings for damage appraisal or injury evaluation.
- Predictive Analytics: AI models will forecast claim outcomes and customer behavior, enabling proactive interventions that reduce fraudulent claims or accelerate settlements.
- Personalized Claims Experiences: AI-driven insights will tailor claims communication and support to individual claimant preferences and histories, boosting satisfaction and loyalty.
- Regulatory & Ethical AI Use: As AI becomes more embedded, insurers and regulators will collaborate to establish transparent and fair AI practices—addressing issues like algorithm bias, accountability, and consumer data rights.
Additionally, AI-powered digital twins and simulation models will help insurers test claims process improvements virtually before real-world implementation, minimizing risks.
By 2025 and beyond, AI will not only automate but also augment claims processing—empowering insurers with smarter decision-making tools that maintain fairness, efficiency, and compliance.
Practical Tip:
Stay informed about AI regulatory developments and prioritize building explainable AI models to foster trust among regulators and customers alike.
Conclusion
AI in insurance isn’t just a tech buzzword—it’s a game-changer for claims processing and fraud detection. By automating workflows and enhancing accuracy, insurers can save time, cut costs, and provide better service. WildnetEdge stands as a trusted partner in deploying these cutting-edge AI solutions tailored to the insurance sector. Ready to transform your claims process? Partner with WildnetEdge and lead the way in insurance innovation.
FAQs
Q1: How does AI improve claims fraud detection in insurance?
AI analyzes vast data sets to identify unusual patterns and behaviors indicative of fraud, enabling early detection and reducing false claims.
Q2: What tasks in claims processing can AI automate?
AI can automate data extraction, claim validation, risk assessment, and customer communications, speeding up the entire claims lifecycle.
Q3: What challenges do insurers face when integrating AI for claims automation?
Common challenges include data quality issues, legacy system compatibility, workforce training, and ensuring compliance with regulations.
Q4: How will AI trends shape the future of insurance claims handling?
AI will enable more predictive, personalized claims resolutions with greater accuracy while ensuring ethical and regulatory standards.
Q5: Why choose WildnetEdge for AI-driven insurance claims solutions?
WildnetEdge offers customized AI platforms designed for insurance providers, combining deep industry knowledge with advanced technology expertise.

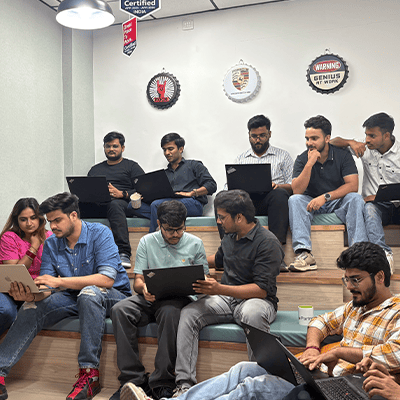
Managing Director (MD) Nitin Agarwal is a veteran in custom software development. He is fascinated by how software can turn ideas into real-world solutions. With extensive experience designing scalable and efficient systems, he focuses on creating software that delivers tangible results. Nitin enjoys exploring emerging technologies, taking on challenging projects, and mentoring teams to bring ideas to life. He believes that good software is not just about code; it’s about understanding problems and creating value for users. For him, great software combines thoughtful design, clever engineering, and a clear understanding of the problems it’s meant to solve.
 sales@wildnetedge.com
sales@wildnetedge.com +1 (212) 901 8616
+1 (212) 901 8616 +1 (437) 225-7733
+1 (437) 225-7733





 ChatGPT Development & Enablement
ChatGPT Development & Enablement Hire AI & ChatGPT Experts
Hire AI & ChatGPT Experts ChatGPT Apps by Industry
ChatGPT Apps by Industry ChatGPT Blog
ChatGPT Blog ChatGPT Case study
ChatGPT Case study AI Development Services
AI Development Services Industry AI Solutions
Industry AI Solutions AI Consulting & Research
AI Consulting & Research Automation & Intelligence
Automation & Intelligence